Odds are, you or someone you know has diabetes. It certainly pays to reinforce what you know about this disease – and to take stock of the lifestyle changes you can make to manage it.
Diabetes is New Zealand’s fastest growing chronic health problem, with nearly 300,000 affected by the disease. It’s estimated another 500,000 people have pre-diabetes.
People with type 2 diabetes are two to four times more likely to develop cardiovascular disease than people who don’t have the disease; and they are more than twice as likely to have a heart attack or stroke.
But it’s not all doom and gloom – controlling blood glucose levels and maintaining a healthy lifestyle can signficantly reduce the complications associated with type 2 diabetes. Research shows you don’t have to be a saint to make a difference to your health, either. These five changes will well and truly have you on your way.
1. Switch to low-GI carbohydrates
Low-GI carbohydrates are slowly digested by the body, meaning they trickle glucose into your bloodstream instead of quickly bursting into your system. Research shows that a low-GI diet can improve blood glucose control in people with type 2 diabetes.
Including just one low-GI carbohydrate at each meal and snack can make a noticeable difference. Low-GI foods include wholegrain bread, pasta, basmati rice, apples, pears and low-fat yoghurt.
Search this website for more information on low-GI foods, or visit www.glycemicindex.com to find the GI values of specific foods. Look for foods with a glycaemic index of 55 or less.
2. Eat at least two serves of wholegrains daily
Upping your intake of whole grains is a must for people with type 2 diabetes.
Researchers are still not 100 per cent sure why whole grains help in the management of type 2 diabetes, though it’s thought to be linked to the insoluble fibre and magnesium they contain.
One serve of whole grains is equal to two slices of wholegrain bread, one cup cooked wholemeal pasta, half a cup natural muesli, 20g popcorn or one cup cooked brown rice. Eat at least two serves of whole grains daily.
3. Get active for at least two-and-a-half hours each week
Frequent exercise is one of the best ways to lower blood glucose levels. Exercise also improves your insulin sensitivity by enhancing the way your skeletal muscles absorb glucose.
According to the American Diabetes Association (ADA), anyone with type 2 diabetes should participate in at least 150 minutes of moderate intensity physical activity, or at least 90 minutes of vigorous activity, each week to improve glycaemic control, assist with weight management and reduce the risk of cardiovascular disease. The ADA also recommends that this exercise be distributed over at least three days of the week, with no more than two consecutive days without physical activity. This equates to a minimum of 22 minutes of moderate-intensity exercise each day.
Weight-loss aside, US research shows that more than four hours of exercise each week can result in a significant reduction in the risk of diabetes for people with pre-diabetes. Most importantly, if people with type 2 diabetes make exercise a regular part of their life, their risk of early mortality decreases substantially.
4. Exercise with weights – three times a week
Just like aerobic exercise, resistance training improves both insulin sensitivity in the muscles and blood glucose control. Research shows that resistance training increases lean muscle mass, which is associated with a decrease in HbA1c (a measure of a person’s average glucose levels over the previous two to three months).
People with well-controlled type 2 diabetes will ideally engage in resistance exercise that targets all major muscle groups three times per week. The ADA recommends three sets of eight to 10 repetitions for each muscle group, using a weight heavy enough that your muscles are fatigued after eight to 10 repetitions.
5. Lose weight (even a little can make a big difference)
Fortunately, you don’t need to lose a huge amount to improve your health – just five to nine kilos will help. Losing weight is probably the best thing you can do to manage your type 2 diabetes. Excess weight increases the body’s resistance to insulin, making it harder to control blood glucose levels. Losing weight can increase the body’s sensitivity to insulin, and reduce your likelihood of developing heart disease and certain types of cancer. It has also been shown that moderate weight-loss can reduce both high blood pressure and glucose levels, as well as improve blood cholesterol levels, which just goes to show how important a small reduction in weight can be.
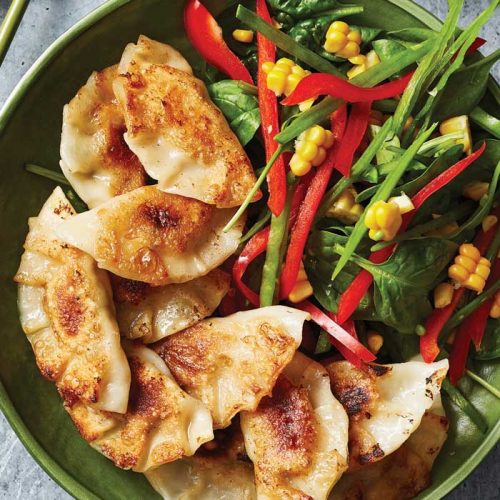
Step-by-step: Building a healthy diabetes-friendly meal
You can make almost any meal – including pizza, pasta and lasagne – diabetes-friendly. Just portion your ingredients following the lists below and away you go!
1. Give vegetables a leading role
There needs to be at least two serves of vegetables in your meal. One serve of vegetables is equivalent to half a cup of cooked vegetables or one cup of salad (not including starchy vegetables such as potato or kumara).
To reach your meal vegetable quota, add lots of grated vegetables to sauces, soups and baked dishes, dish up your meal with a generous serve of steamed green vegetables, or make veges the ‘star’ of dinner rather than a side dish.
- 1 cup* cooked non-starchy vegetables such as broccoli, cauliflower, carrot etc.
- 2 cups* salad such as lettuce, spinach, tomato, capsicum etc.
*These quantities are the minimum to aim for – feel free to load up your plate!
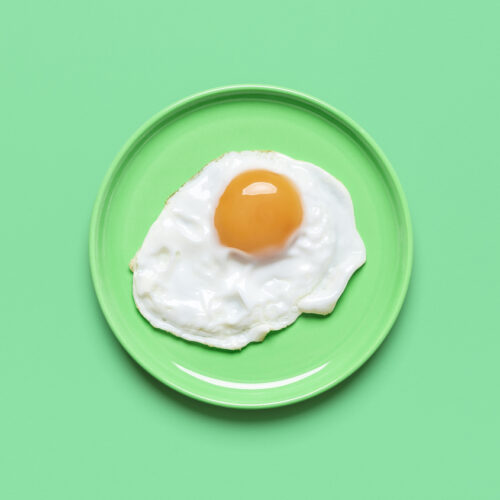
2. Add a portion of lean protein
Protein is an important part of a diabetes-friendly meal because it helps to lower the total GI of the overall meal (protein foods are generally low-GI because they contain minimal carbohydrates). Proteins also help you feel full for longer. Always choose reduced-fat dairy products and lean meat, and remove all visible fat prior to cooking.
- 2 small (45g) eggs
- 120g tofu
- 100g cooked skinless chicken (125g raw)
- 100g cooked lean beef, lamb or pork (125g raw)
- 120g cooked fish (170g raw) including canned tuna, salmon and mackerel
- 40g (about 2 slices) reduced-fat cheese
- 1/2 cup cooked lentils, chickpeas or 3-bean mix
3. Choose moderate amounts of carbohydrates
Keep the glycaemic load of your meal down by choosing smaller portions of starchy vegetables. Using low to moderate-GI carbohydrate foods will help keep the overall GI of the meal low. Choose pasta, noodles, basmati rice, pearl barley, quinoa, grainy breads and legumes.
Don’t forget that legumes contain low-GI carbohydrates as well as protein (see protein above), so be mindful of that when you’re creating your meal.
Carbohydrates
1 cup cooked pasta or noodles, preferably wholemeal
1 small whole grain bread roll
2 slices whole grain bread
1 cup cooked couscous
3/4 cup cooked brown rice or basmati rice
3/4 cup quinoa
1 cooked small potato
1 cooked medium kumara
1 medium corn cob
4. Add a little healthy fat
Like protein, healthy fats help lower the GI of the overall meal. Good fats are also important for keeping cholesterol levels in check. Aim for only small quantities of healthy fats such as olive oil, avocado and nuts or seeds.
NOTE: Adding fat is not always necessary as many sources of protein – such as meat and tofu – can provide ample fat.
- 2 teaspoons pesto
- 1 teaspoon plant-based oil (eg. olive oil)
- 2 teaspoons crushed or sliced nuts
- 10g avocado
- 1 tablespoon hummus
- 2 teaspoons salad dressing
What a healthy plate looks like
Before dishing up your meal, mentally divide your plate into four quarters. One quarter should contain protein foods, another quarter should contain low to medium-GI carbohydrate foods and the rest of your plate (the final half) should be filled with vegetables and/or salad. This will help you get the right balance to your meal and help with portions sizes. Remember, smaller plates make for smaller portion sizes.
And finally…
Most people think of reducing sugar when they are cooking for someone with diabetes. While this is something you need to consider, there are a few other things to keep in mind, too.
Boost the fibre
Add fibre by including vegetables, beans and legumes where possible (but especially in sauces, soups and salads), and choose wholegrain or wholemeal varieties of breads, cereals and pastas.
Reduce the saturated fat
To help keep the overall kilojoules down, trim any visible fat from meat, remove skin from chicken, choose low-fat versions of all dairy foods, and minimise total fat whenever possible.
‘Pass’ on the salt
Cook with low-salt, salt-reduced or no-added-salt ingredients, especially when it comes to canned vegetables, canned legumes, and stock. Choose foods canned in spring water rather than brine, and don’t add salt to the food.
The difference
- Type 1 diabetes is an autoimmune disease where the body has destroyed the insulin-producing cells in the pancreas. Therefore, the body is unable to produce insulin and regular insulin injections must be given.
- Type 2 diabetes is generally caused by lifestyle and occurs when the insulin produced does not work properly, or the body cannot produce enough insulin to maintain normal blood glucose levels. Over 90 per cent of people with diabetes have type 2.
Can you reverse type 2 diabetes?
Type 2 diabetes cannot be reversed but the right diet, exercise and weight-loss can make blood glucose control easier. In fact, in over 50 per cent of people, blood glucose levels can be normalised by:
- following a kilojoule-controlled diet
- increasing physical activity
- losing some weight.
What about pre-diabetes?
Pre-diabetes is a condition when cells in the body are becoming insulin resistant and blood glucose levels are higher than they should be, but are not high enough to be classified as diabetes. For those diagnosed with pre-diabetes, taking steps to improve insulin resistance (such as eating a healthy and balanced diet, losing weight and participating in regular physical activity), may be enough to avoid ever being diagnosed with type 2 diabetes.
www.healthyfood.com