Diverticular disease is one of the most common health problems in the West, affecting up to 65 per cent of people over 85 years old and around 5 per cent of people aged under 40, yet many of us have never even heard of it. And now it’s on the rise in younger populations. HFG lifts the lid on this common intestinal condition.
Here’s what we cover:
Cramping, bloating and diarrhoea are all gut symptoms that can be linked to anything from food intolerances to gastro. But if the discomfort rapidly develops from mild to severe, diverticulitis might prove to be the culprit.
Diverticulitis develops from diverticulosis, a common condition where small pockets or pouches form in the wall of the large intestine. Worldwide, diverticular disease has the highest incidence in the US, Western Europe and Australia, affecting up to 50 per cent of the population aged 60 and above. And recent reviews show it’s on the rise in people aged 18 to 64 years.
What is diverticular disease?
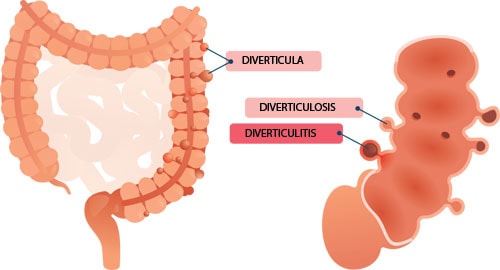
‘Diverticulum’ is a medical term based on the Latin word for a byway or diversion from the normal pathway. What it describes are small, bulging pouches in the lining of the gastrointestinal tract. Think of these not as holes, but small hollows in the wall of the bowel. The majority of these bulges (called diverticula) do not cause any symptoms and are often only found by coincidence during an examination being performed for some other medical condition, like a routine colonoscopy.
When these bulges exist with no pain or symptoms, the condition is known as diverticulosis. However, when faeces and food particles get caught in these pockets and cause them to become infected or inflamed, the condition is called diverticulitis. Symptoms often include crampy pain and tenderness, usually in the left side of the lower abdomen, and possibly nausea. Depending on the severity of the infection, you may also experience a fever, chills and fatigue.
Collectively, diverticulosis and diverticulitis are known as diverticular disease.
Common causes of diverticular disease
The two main reasons for these pouches forming are ageing and a low-fibre intake. The chance of developing diverticular disease increases with age, and nearly everybody over the age of 80 will have developed some level of the condition.
As for fibre intake, a low-fibre diet contributes to small, infrequent bowel movements and constipation. When stools become hard and dry, this causes straining and overly forceful contractions, putting pressure on the muscular wall of the large intestine, which can then force the bowel lining to bulge through any weak spots.
When things get serious
Most bulges are small, ranging from 3mm to just over 3cm in diameter, and rarely require treatment. Very occasionally, however, inflamed pouches can rupture and require immediate surgery. Sometimes an infection can cause damaged tissue from neighbouring organs to stick together, forming a fistula or abnormal opening, which also requires immediate medical attention.
What’s happening in your large intestine
Signs of diverticular disease
While most people are asymptomatic, some people experience the following symptoms:
- Abdominal pain
- Bloating
- Constipation
- Diarrhoea
- Blood in stools.
Symptoms of an acute infection, or diverticulitis, include:
- Severe pain
- Nausea
- Loss of appetite
- Fever
- Chills or night sweats
- Bleeding and changes in bowel habits.
Treatment for acute diverticulitis
Acute diverticulitis often requires a visit to your GP who, depending on the severity, may advise bowel rest – liquid only intake – for a few days. You may also need antibiotics to fight off infection or even need to be admitted to hospital.
During a flare-up, a low-fibre intake will be advised to prevent further irritation and allow the bowel to heal. This means eating easily digested foods such as white bread and rice, and avoiding fibrous foods like seeds, nuts, legumes and the skin on fruits and vegetables. Quite the opposite of our usual healthy-eating advice! It’s also best to avoid raw foods, especially salads, and opt for soft or cooked vegetables and fruit instead.
As inflammation eases, you’ll be advised to gradually wean yourself back onto a higher fibre intake to help make your bowel movements more comfortable and prevent constipation and more pouches from developing. You may be recommended products like psyllium husks (Metamucil) to help increase stool volume.
Foods like yoghurt and kefir, which contain protective probiotics, may also be of benefit, especially if you’re taking antibiotics to help treat infection. Consuming probiotic-rich foods can help you re-establish healthy bacteria in your intestine.
Your GP may also recommend you visit a qualified dietitian to assist in devising a personalised food management strategy.
Managing diverticulosis with diet
Most people with diverticulosis don’t require any treatment other than increasing their dietary fibre intake to increase stool bulk and softness, and to promote regularity.
Consuming a decent amount of water or other liquids, upwards of two litres a day, to help produce a soft stool is also important. Avoid becoming constipated as this increases the risk of a flare-up. When you need to do a number two, don’t hold on – always respond to your body’s urge for bowel movements.
What you can and can’t eat
Many people are told to avoid certain foods that can irritate the bowel wall. These include:
- Nuts and seeds
- Popcorn
- Fruits with seeds (such as strawberries, raspberries and figs)
- Vegetables with seeds (such as cucumbers, tomatoes and corn).
While most people with diverticular disease can eat these foods, some may find they cause problems, especially in large amounts. To be on the safe side, avoid them if you have diverticular disease. Consuming at least 30g of fibre a day not only reduces your risk of developing diverticulitis, it boosts gut function and optimises overall health.
Get more of these 3 fibre types
Most of us could benefit from including more fibre in our daily diet. Eating more fibre means getting a balance of the three different types:
- Boost soluble fibre by including more oats, barley, psyllium husks, seeds (if you tolerate them) and lentils in your daily meals.
- Boost insoluble fibre by choosing to eat wholegrain bread and cereal products, rice bran, the skin of fruit and more vegetables and nuts (if you tolerate them).
- Boost resistant starch intake by eating more chickpeas, red kidney beans, navy beans and other legumes, cooked and cooled potatoes and pasta, as well as under-ripe bananas.
A high-fibre day on a plate
Breakfast
Bowl of porridge or Bircher muesli with sliced banana
Lunch
Dinner
Fish with potato salad and slaw (or veg such as carrots and broccoli)
Snacks
Fresh fruit, nuts (if you can tolerate them), homemade muesli bars
What’s the deal with resistant starch?
Fermentation of resistant starch in the bowel produces the short-chain fatty acid, butyrate. This strengthens the lining of the large bowel and reduces the risk of diverticular disease and other diseases of the digestive tract.
Article sources and references
- Aune D et al. 2020. Dietary fibre intake and the risk of diverticular disease: a systematic review and meta-analysis of prospective studies. Eur J Nutr. 59(2): 421-432.https://pubmed.ncbi.nlm.nih.gov/31037341/
- Crowe F et al. 2011. Diet and risk of diverticular disease in Oxford cohort of European prospective investigation into cancer and nutrition. BMJ. 343: d4131.https://pubmed.ncbi.nlm.nih.gov/21771850/
- Crowe F et al. 2014. Source of dietary fibre and diverticular disease incidence: a prospective study of UK women. Gut. 63(9): 1450-1456.https://pubmed.ncbi.nlm.nih.gov/24385599/
- You H et al. 2019. The management of diverticulitis: a review of the guidelines. Med J Aust. 211(9): d10.5694.https://www.mja.com.au/journal/2019/211/9/management-diverticulitis-review-guidelines
- McSweeney W & Srinath H. 2017. Diverticular disease practice points. Australian Family Physician. 46(11): 829-832.https://pubmed.ncbi.nlm.nih.gov/29101918/
- Strate L et al. 2008. Nut, corn, and popcorn consumption and the incidence of diverticular disease. JAMA. 300(8): 907-14.https://pubmed.ncbi.nlm.nih.gov/18728264/
- Weizman A & Nguyen G. 2011. Diverticular disease: epidemiology and management. Canadian Jr Gastr. 25(7): 385–389.https://jhu.pure.elsevier.com/en/publications/diverticular-disease-epidemiology-and-management-4
www.healthyfood.com